Radioembolization
Radioembolization (Yttrium-90) is very similar to chemoembolization but with the use of radioactive microspheres. This treatment incorporates the radioactive isotope Yttrium-90 into the embolic spheres to deliver radiation directly to the tumor. Each sphere is about the size of five red blood cells in width. These beads are injected through a catheter. The beads become lodged within the tumor vessels where they exert their local radiation that causes cell death. This technique allows for a higher, local dose of radiation to be used, without subjecting healthy tissue in the body to the radiation. The Yttrium-90 radiates from within and, since it is administered in the hepatic artery, it can be viewed as “internal” radiation.
Radioembolization is a palliative, not a curative, treatment-but patients benefit by extending their lives and improving their quality of life. It is a relatively new therapy that has been effective in treating primary and metastatic liver cancers. It is performed as an outpatient treatment. There are fewer side effects from this treatment compared to standard cancer treatments, with the main one being fatigue for seven to 10 days.
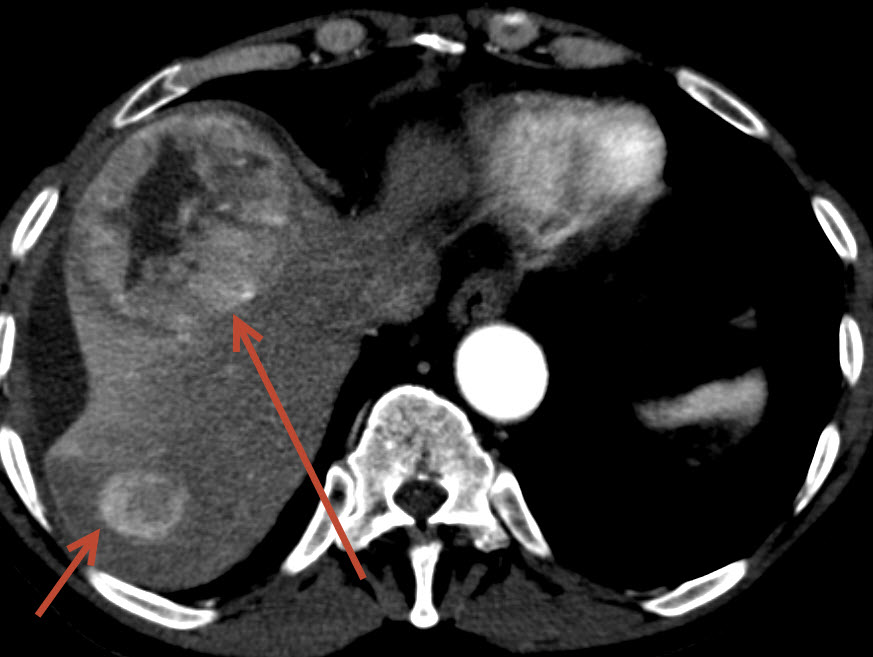
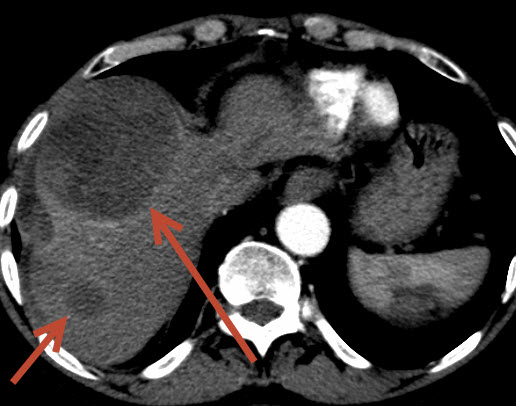
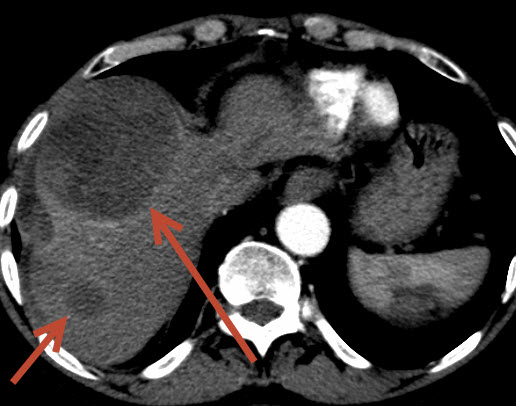
The Images above show a 64 year old male with a heart transplant treated at FIS for liver cancer. One drug used in chemoembolization has possible cardiac side effects, given this, radioembolization was chosen for treatment. The pretreatment images show two large tumors in the right lobe of the liver (left side of the picture-arrow) to be bright suggesting high blood flow, common in this type of tumor. After one radioembolization treatment, the follow-up CT demonstrates the entire tumor to be dark and necrotic (dead) without any new tumors. The patient complained of mild fatigue for one month but had no other side effects.
Radioembolization requires two outpatient visits to the hospital. The first procedure is 2-3 hours and is aimed at decreasing complications. This procedure entails “mapping” out the anatomy of the arteries to the liver by injecting contrast in the liver arteries through a catheter from the groin. Any arteries that are not feeding directly to the liver are blocked with tiny coils to prevent the radioactive beads from floating to areas outside the liver. During the first procedure a “test dose” of radiation is directly infused into the liver artery that does not injure the tumor or the liver, but it assures the radiation does flow into the tumor and remains there. If the “test dose” of radioactive beads flow through the tumor and into the body, this test will demonstrate it. Approximately one week after the first “mapping” procedure and test radiation dose, the treatment dose of radiation is given. Both visits are typically outpatient procedures and patients are home in the early afternoon. Neither requires a long recovery or bed rest, at home or in the hospital.
THE SERVICES LISTED ON THIS WEBSITE ARE FOR GENERAL INFORMATION PURPOSES ONLY AND DO NOT INCLUDE ALL SERVICES OF FLORIDA INTERVENTIONAL SPECIALISTS. WHILE WE STRIVE TO KEEP THE INFORMATION UP TO DATE AND CORRECT, WE MAKE NO REPRESENTATIONS OR WARRANTIES OF ANY KIND, EXPRESS OR IMPLIED, ABOUT THE CONTENT, COMPLETENESS, ACCURACY, RELIABILITY, LEGALITY, SUITABILITY OR AVAILABILITY, WITH RESPECT TO THE SERVICES CONTAINED ON THIS WEBSITE.

