Abdominal Aortic Aneurysm
The experience of endovascular repair of thoracic and abdominal aortic aneurysms by the FIS physicians at TGH began in 1996, far earlier than the procedure was established as mainstream treatment. We have been involved in a multitude of clinical trials for many different devices and host training courses for industry to train other physicians from around the country on the proper use of their devices and advanced techniques. We have performed over 1000 thoracic (TEVAR) and abdominal (EVAR) endovascular repairs of aneurysms.
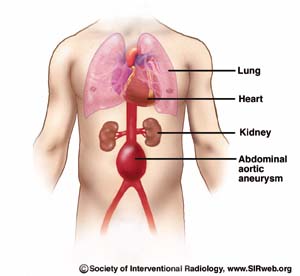
Interventional Radiologists offer a minimally invasive procedure without open surgery to treat Abdominal Aortic Aneurysms. An Abdominal Aortic Aneurysm (AAA) is a weak area in the aorta, the main blood vessel that carries blood from the heart to the rest of the body. As blood flows through the aorta, the weak area bulges like a balloon and can burst if the balloon gets too big.
In the past 30 years, the occurrence of Abdominal Aortic Aneurysms (AAA) has increased threefold. AAA is caused by a weakened area in the main vessel that supplies blood from the heart to the rest of the body. When blood flows through the aorta, the pressure of the blood beats against the weakened wall, which then bulges like a balloon. If the balloon grows large enough, there is a danger that it will burst. Most commonly, aortic aneurysms occur in the portion of the vessel below the renal (kidney) artery origins. The aneurysm may extend into the vessels supplying the hips and pelvis.
Once an aneurysm reaches 5 cm in diameter, it is usually considered necessary to treat to prevent rupture. Below 5cm, the risk of the aneurysm rupturing is lower than the risk of conventional surgery in patients with normal surgical risks. The goal of therapy for aneurysms is to prevent them from rupturing. Once an abdominal aortic aneurysm has ruptured, the chances of survival are low, with 80 to 90 percent of all ruptured aneurysms resulting in death. These deaths can be avoided if an aneurysm is detected and treated before it ruptures.
AAA Prevalence
- Approximately one in every 250 people over the age of 50 will die of a ruptured AAA
- AAA affects as many as eight percent of people over the age of 65
- Males are four times more likely to have AAA than females
- AAA is the 17th leading cause of death in the United States, accounting for more than 15,000 deaths each year.
- Those at highest risk are males over the age of 60 who have ever smoked and/or who have a history of atherosclerosis (“hardening of the arteries”)
- 50 percent of patients with AAA who do not undergo treatment die of a rupture
Smoking is a Major Risk Factor for AAA and other Vascular Disease
- Those with a family history of AAA are at a higher risk (particularly if the relative with AAA was female)
- Smokers die four times more often from ruptured aneurysms than nonsmokers
AAA Symptoms
AAA is often called a “silent killer” because there are usually no obvious symptoms of the disease. Three out of four aneurysms show no symptoms at the time they are diagnosed. When symptoms are present, they may include:
- Abdominal pain (that may be constant or come and go)
- Pain in the lower back that may radiate to the buttocks, groin or legs
- The feeling of a “heartbeat” or pulse in the abdomen
Once the aneurysm bursts, symptoms include:
- Severe back or abdominal pain that begins suddenly
- Paleness
- Dry mouth/skin and excessive thirst
- Nausea and vomiting
- Signs of shock, such as shaking, dizziness, fainting, sweating, rapid heartbeat and sudden weakness
AAA Diagnosis
In some, but not all cases, AAA can be diagnosed by a physical examination in which the doctor feels the aneurysm as a soft mass in the abdomen (about the level of a belly button) that pulses with each heartbeat.
The most common test to diagnose AAA is ultrasound, a painless examination in which a device (a transducer) about the size of a computer mouse is passed over the abdomen. Sound waves are computerized to create “pictures” of the aorta and detect the presence of AAA. Other methods for determining the aneurysms’ size are CT scan (computerized tomography), MRI (magnetic resonance imaging), and arteriogram (real time x-rays).
AAA Treatments
Currently, there are three treatment options for AAA:
Surveillance – Small AAA’s (less than 5 centimeters or about 2 inches), which are not rapidly growing or causing symptoms, have a low incidence of rupture and often require no treatment other than “watchful waiting” under the guidance of a vascular disease specialist. This typically includes follow-up ultrasound or CT exams at regular intervals to determine if the aneurysm has grown.
Surgical Repair – This procedure involves an incision from just below the breastbone to the top of the pubic bone by a vascular surgeon. The surgeon then clamps off the aorta, cuts open the aneurysm and sews in a graft to act as a bridge for the blood flow. The blood flow then goes through the plastic graft and no longer allows the direct pulsation pressure of the blood to further expand the weak aorta wall.
Interventional Repair – This minimally invasive technique is performed by an interventional radiologist using imaging to guide the catheter and graft inside the patient’s artery. For the procedure, an incision is made in the skin at the groin through which a catheter is passed into the femoral artery and directed to the aortic aneurysm. Through the catheter, the physician passes a stent graft that is compressed into a small diameter within the catheter. The stent graft is advanced to the aneurysm, then expanded or opened creating new walls in the blood vessel through which blood flows and also cutting off the blood supply to the aneurysm.
This is a less invasive method of placing a graft within the aneurysm to redirect blood flow and stop direct pressure from being exerted on the weak aortic wall. This relatively new method eliminates the need for a large abdominal incision. It also eliminates the need to clamp the aorta during the procedure. Clamping the aorta creates significant stress on the heart, and people with severe heart disease may not be able to tolerate this major surgery. Stent grafts are most commonly considered for patients at increased surgical risk due to age or other medical conditions.
The stent graft procedure is not for everyone, though. It is still a new technology and we don’t yet have data to show that this will be a durable repair for long years. Thus, people with a life expectancy of 20 or more years may be counseled against this therapy. It is also a technology that is limited by size. The stent grafts are made in certain sizes, and the patient’s anatomy must fit the graft, since grafts are not custom-built for each patient’s anatomy.
Second Opinion
In order to determine if you are a candidate for the interventional radiology procedure, it’s best to get a second opinion from an interventional radiologist. You can ask for a referral from your doctor, call the radiology department of any hospital and ask for interventional radiology or visit the doctor finder link at the top of this page to locate a doctor near you.
A stent-graft is threaded into the blood vessel where the aneurysm is located. The stent graft is expanded like a spring to hold tightly against the wall of the blood vessel and cut off the blood supply to the aneurysm.
Efficacy and Patient Safety
Interventional repair is an effective treatment that can be performed safely, resulting in lower morbidity and lower mortality rates than those reported for open surgical repair.
Recovery Time
- Patients are often discharged the day after interventional repair, and typically do not require intensive care stay post-op
- Once discharged, most return to normal activity within 2 weeks compared to 6-8 weeks after surgical repair
Benefits of Interventional Repair
- No abdominal surgical incision
- No sutures, or sutures only at the groins
- Faster recovery, shorter time in the hospital
- No general anesthesia in some cases
- Less pain
- Reduced complications
Disadvantages of Interventional Repair
- Possible movement of the graft after treatment, with blood flow into the aneurysm and resumption of risk of growth/rupture of the aneurysm
- Probable life-time requirement for follow-up studies to be sure the stent graft is continuing to function
THE SERVICES LISTED ON THIS WEBSITE ARE FOR GENERAL INFORMATION PURPOSES ONLY AND DO NOT INCLUDE ALL SERVICES OF FLORIDA INTERVENTIONAL SPECIALISTS. WHILE WE STRIVE TO KEEP THE INFORMATION UP TO DATE AND CORRECT, WE MAKE NO REPRESENTATIONS OR WARRANTIES OF ANY KIND, EXPRESS OR IMPLIED, ABOUT THE CONTENT, COMPLETENESS, ACCURACY, RELIABILITY, LEGALITY, SUITABILITY OR AVAILABILITY, WITH RESPECT TO THE SERVICES CONTAINED ON THIS WEBSITE.
